Special situations: Breastfeeding after adoption or breast surgery
“Can you breastfeed after implants?” When you’re hanging out with other new moms or moms-to-be, all kinds of topics get discussed and debated, whether it’s a great new nursing bra, the real deal of being in your third trimester, getting more sleep, challenges with your partner or worries about your baby’s health. (We can likely thank Kourtney Kardashian for that “breastfeeding after implants” chat.)
The answer, by the way, is that yes, you can almost certainly breastfeed if you have breast implants. In many cases, you can also breastfeed after breast reduction surgery (known as BFAR). You can even breastfeed, in some circumstances, a baby that you have adopted or has been born via a surrogate. That’s right: Breasts are amazing.
“I think people have become much more aware of the possibility of breastfeeding in many kinds of circumstances that no one dreamed were possible twenty years ago,” says Diana West , an International Board Certified Lactation Consultant (IBCLC) in northern New Jersey. “There is also much more understanding now that you don’t have to have a full milk supply in order to have a satisfying breastfeeding experience, and every drop of human milk is precious for a child.”
Check out more info on breastfeeding in special circumstances…chances are it could apply to someone you know or even you!
Breastfeeding after implants
Experts say mothers with breast implants (also known as breast augmentation) usually can breastfeed, although they may have a smaller supply of breast milk. Success usually depnds on three factors:
-
Where the breast was cut during the surgery
Despite a lack of enough research to determine the absolute best location of the incision, it seems to be an incision under the breast or in the armpit is less likely to affect milk ducts, nerves and breast function than an incision made around the areola (the colored skin around the nipple). -
Where the implant was placed
An implant placed directly under the glandular tissue puts pressure on the tissue, which can lead to reduced milk flow. An implant under the chest muscle is less likely to cause this pressure. -
The kind of breast tissue you have
And finally, the kind of breasts you had before having your breast implant surgery can impact your ability to exclusively breast feed. If, for example, your breasts were widely spaced (more than 1.5 inches of flat space between them) tubular-shaped, underdeveloped or different sizes before the surgery, that may point to insufficient glandular tissue, which would affect milk supply even before surgery took place. (Of course, the vast majority of women with small breasts can make enough breast milk for their babes.)
Source:
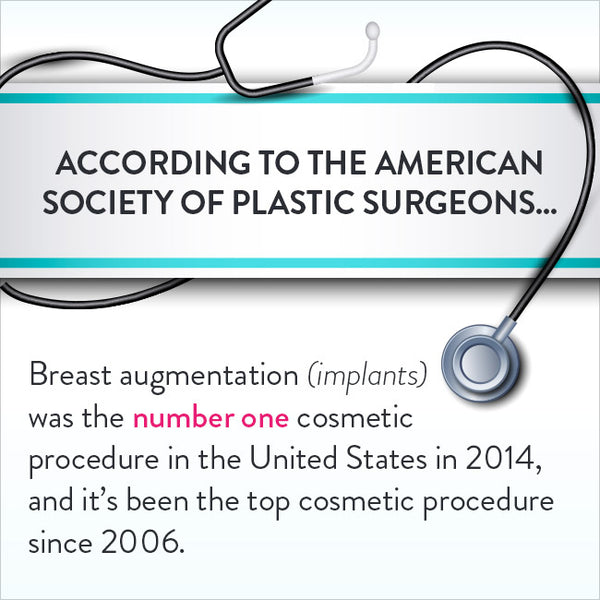
2014 Plastic Surgery Statistics Report
Some moms have concerns about silicon from the implants entering their breast milk, but MotherRisk researchers at the Hospital for Sick Children in Toronto, Canada, found that silicon levels were not higher in the breast milk or blood of women with implants.
Source:
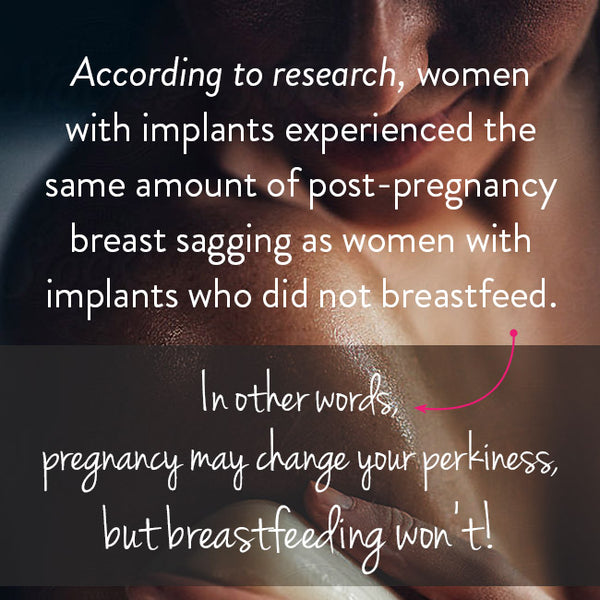
The Effect of Breastfeeding on Breast Ptosis Following Augmentation Mammaplasty
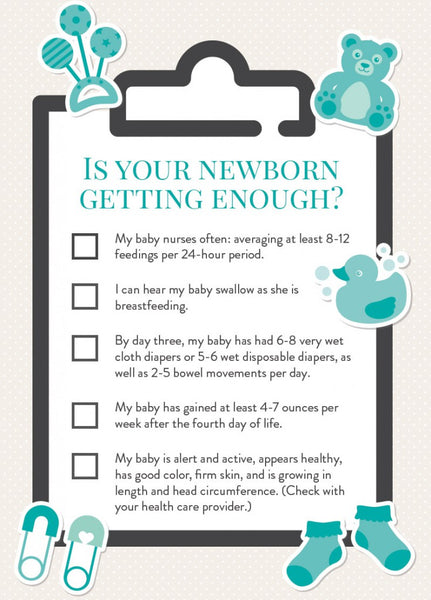
Bottom line: Like any new breastfeeding mom, breastfeed as much as possible in the early weeks to establish your supply, and keep track of your baby’s pees and poops, which indicate your little one is getting enough milk. If your milk supply is low, you can work with an IBCLC to increase it.
Source:
La Leche League International
Breastfeeding after breast reduction surgery
Breastfeeding after breast reduction surgery (BFAR) is also doable for many moms. Breast reduction is one of the most frequently performed operations by plastic surgeons. It is more invasive than a breast augmentation, and because nerves and ducts have been cut, it’s going to have more of an impact on milk supply. As the technique used by your surgeon is key to your success at breastfeeding, talk to your surgeon, or get a copy of your surgical report. Best chances for making enough milk is when your nipple was not completely severed and the lower part of your nipple and areola were kept intact.
Breastfeed as often as possible in the first few weeks to establish milk supply, and work with your health care provider or IBCLC to make sure your baby is getting enough. Your IBCLC will also have ideas on increasing milk supply through pumping or galactagogues (foods or herbs that may boost milk production). You can supplement with a nursing system that uses a tiny tube placed alongside the breast to deliver additional volume right along with the breast milk you’re producing.
Hollie Hauptly, a mom and birth doula in Grapevine, Texas, had breast reduction surgery as a teenager and experienced quite different breastfeeding situations with each of her three kids. For her first child, she struggled initially. “After accepting the fact that our breastfeeding routine would be different than I had envisioned, we developed our new normal—breastfeed, bottle feed formula, wait 30 minutes and pump for about 15 minutes to encourage supply, repeat,” says Hauptly, who blogged about her experience with her first two children at Birth Boot Camp.
For her second child, she felt much more prepared and made some key changes: nursing on demand rather than on a schedule, more skin-to-skin contact and using galactagogue products. This time, she breastfeed her daughter exclusively, no supplementing required.
For her third child, things were rocky for the first two months, because he was born with a severe tongue and lip tie, which meant it was tough to get a good latch and her supply dropped. They got back on track by working with two IBCLCs and using a nipple shield for the latch issues. Now that her son is three-and-a-half months old, after breastfeeding she supplements with an ounce or two of donor breast milk, and he’s thriving. “I dreamed of also exclusively breastfeeding this baby but I remind myself that every breastfeeding relationship will be different,” she says. “My biggest piece of advice is to learn as much as you can about your particular situation and get the support of an experienced IBCLC who will help and support you on your breastfeeding journey. Find a local La Leche League group or a moms’ support group. They can be so helpful!”
Breast surgeries by the numbers
In the United States in 2014:
| Breast augmentation (cosmetic) | 286,000 |
| Breast implant removal (augmentation patients) | 23,744 |
| Breast lift | 92,724 |
| Breast reduction (aesthetic patients) | 41,309 |
| Breast implant removal (reconstructive patients) | 17,496 |
| Breast reconstruction* | 102,215 |
| Breast reduction (reconstructive patients) | 59,883 |
*performed by member of ASPS
Source:
2014 Plastic Surgery Statistics Report
Source:
Annals of Surgical Innovation and Research 2009
Breastfeeding after adoption
Breastfeeding without giving birth—whether that means adoption, a baby born by a gestational surrogate, or a two-mom family where both women want to breastfeed—is also an option for many moms. “My stance is that it’s about the nursing, not necessarily about the volume of milk,” says Dolly Smith, an IBCLC and RN who works with adoptive nursing moms through her Seattle, Washington practice, After the Stork. “Nursing is about keeping a baby close and learning to respond easily to baby’s cues. The goal is to create a bond and if milk comes, that’s a bonus.”

Sources:
US State Department
Adoptive Families
There are a number of protocols that an IBCLC who specializes in induced lactation (in a woman who has never been pregnant) or relactation (in a woman who has been pregnant before) can suggest, and they could include pumping well before baby arrives to stimulate production, herbal medications and prescription medications.
“Remember there are multiple ways to do this,” says Smith. “When you research the protocols, you will get a sense—there is no way I will do x, but I will do a and b. Then you work with your lactation consultant to build on what feels right for you.” Like a mom who breastfeeds after a breast reduction, you may use an at-breast supplementer as you nurse. “My biggest tip there is to look beyond the equipment and into your baby’s eyes,” advises Smith.
One last key thing to remember: ask for help from your partner or a loved one. “In any breastfeeding situation, partner support is huge; it’s the number one reason moms will continue to breastfeed,” says Smith. “It does so much mom’s confidence and resolve.”
Good luck and best wishes, mamas…hope you meet your breastfeeding goals!